What Causes Plaque to Build Up in the Arteries – Leading to a Heart Attack – and How to Avoid It
- Jimmy Song
- Jul 2, 2025
- 5 min read
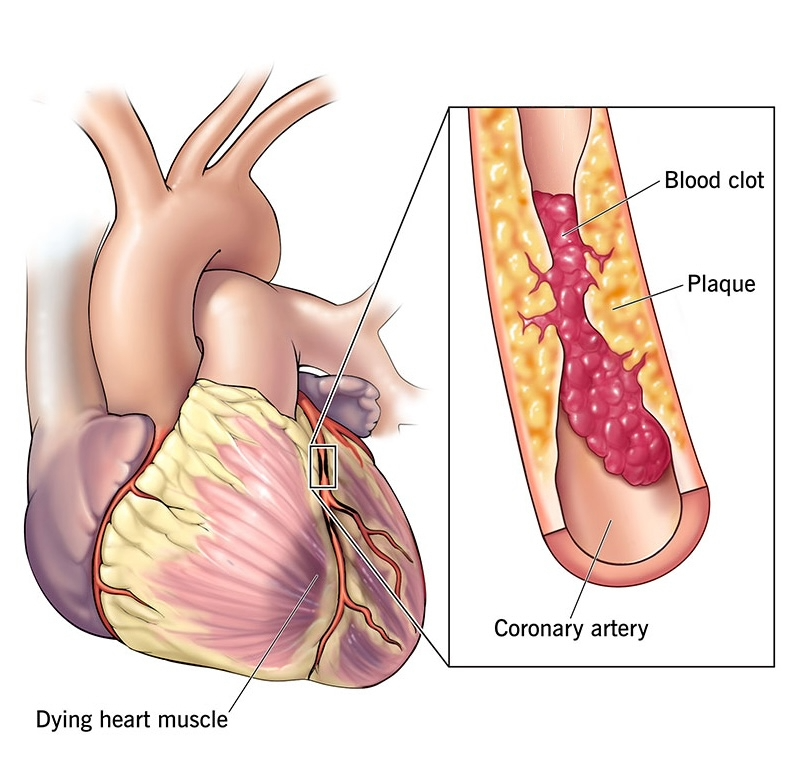
Plaque buildup in the arteries is typically caused by lipoproteins, which carry cholesterol in the blood and can stick to the endothelial (“inner”) lining of the arteries. Why do lipoproteins stick to the inner lining of the arteries? Typically, it’s caused by “endothelial dysfunction”, which is inflammation of the arterial lining. The more inflammation there is in the arterial lining, the more likely lipoproteins – particularly the more harmful low-density lipoproteins (LDL) – are likely to stick to and accumulate there. Cholesterol can also enter the endothelial lining when it is damaged.

But just because LDL cholesterol is present in the blood stream, that does not necessarily mean that it accumulates in the coronary arteries. Inflammation and endothelial dysfunction must be present as well. This is why simple blood cholesterol tests can be misleading at times. High levels of cholesterol or lipoproteins in the blood alone does not immediately or automatically translate to plaque buildup in the arteries. And the absence of cholesterol or lipoproteins in the blood does not necessarily mean plaque buildup does not exist in the arteries. This can create a dangerous situation whereby the patient is given the “all clear” after blood work is done, when in fact risk of a heart attack is quite high due to atherosclerotic plaque buildup in the arteries.

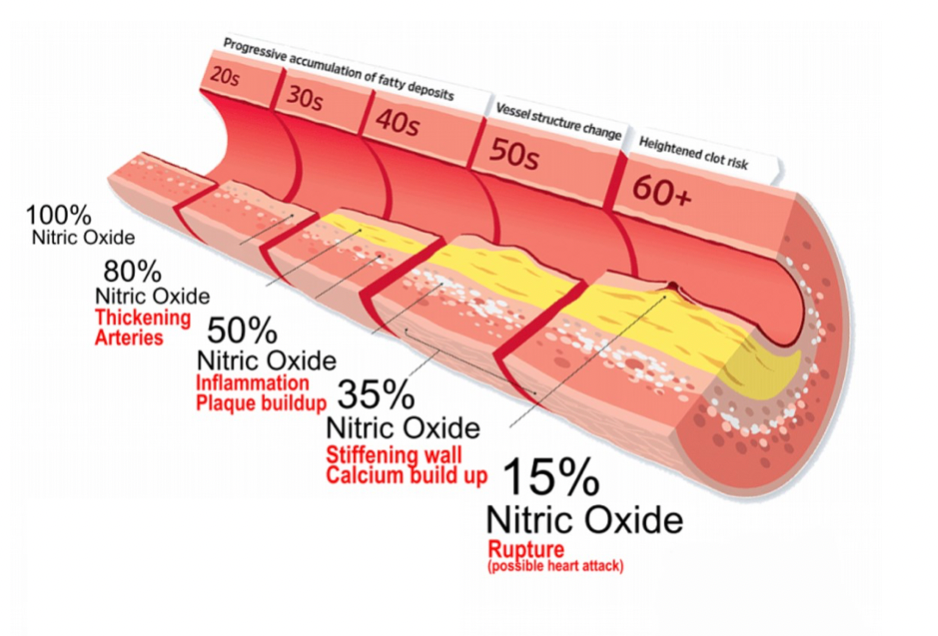
What causes endothelial dysfunction, or inflammation, in the inner lining of the arteries? The main culprits tend to be high blood pressure (“hypertension”), stress, obesity, diabetes, diet (high consumption of sugar or saturated fats), and/or smoking/nicotine consumption. Smoking/nicotine consumption is one of the main drivers of cardiovascular disease and one of the leading preventable causes of death. Aside from causing lung damage, smoking or any nicotine consumption causes inflammation in the endothelial lining of the coronary arteries, thereby leading to plaque buildup. But nicotine also impacts the coronary arteries in another way. It acts to deplete the nitric oxide levels in the endothelial lining. Nitric oxide helps keep the arteries relaxed, flexible and dilated (wide open) for smooth, unobstructed blood flow. When the endothelial cells are depleted of nitric oxide, they become stiff and narrow, making it harder for blood to pass through – increasing the risk of (1) ischemia, (2) a non-obstructive heart attack, or (3) a blood clot causing a fully-obstructive heart attack.
Does high blood pressure (“hypertension”) mean there is plaque buildup (“atherosclerosis”) in the coronary arteries? Not necessarily. But it does mean that it’s likely. What’s most dangerous though, similar to blood cholesterol readings, are those cases where blood pressure presents as normal, however, there is significant plaque buildup in the coronary arteries. This tends to happen frequently with nicotine users. From the outside, they look healthy and display no obvious symptoms of cardiovascular disease. But inside, their arteries have narrowed and stiffened so much that a heart attack is imminent if there is any type of minor obstruction.
Partially driven by smokers, there is a growing percentage of younger heart attack sufferers, i.e. people in their late 30s and 40s versus what we normally assume to be the typical age of a heart attack sufferer (60+ years of age). The younger heart attack sufferers tend not to present standard risk signs, such as high blood pressure, high cholesterol, obesity or diabetes, and yet still suffer preventable heart attacks.
Why It’s Hard to Detect Plaque
Heart attacks can occur unexpectedly because the main driver of risk, atherosclerosis (arterial plaque buildup), is very difficult to detect and measure without expensive, difficult-to-access hospital imaging equipment. Blood pressure and cholesterol readings are just loose proxies for the presence of plaque buildup, but can be misleading because they are not always representative of the underlying reality. Additionally, imaging technologies like ultrasounds and MRIs do not provide sufficient clarity to properly diagnose atherosclerosis.
Finally, coronary artery calcium (CAC) scans can give insights into the presence of hardened plaque in the arteries. But the type of plaque that tends to rupture and cause heart attacks is soft plaques, which are undetected by CAC scans. The best way currently to measure coronary atherosclerosis is through a coronary angiogram or CT angiogram – a highly invasive procedure that also causes a large amount of radiation to be absorbed. Additionally, CT angiograms can’t be repeated often – only maybe once every 5 to 10 years. But in reality, it’s rarely done more than once in a patient’s lifetime. As a result, tracking changes in arterial health over time is very difficult to do.

Plaque buildup in the arteries can take years to build up. But in some cases it can happen very quickly: in some cases just a matter of months – from 0% to 99% blockage. This is driven by genetics and lifestyle factors. Thus, ongoing monitoring of cardiovascular health is absolutely critical.
Prevention
The key to good cardiovascular health – and by extension a longer, higher-quality life – is clean, well-dilated (wide-open), flexible arteries that allow for unrestricted blood flow. This can be facilitated in a number of ways, including:
Regular exercise (raising your heart rate to at least 50% of your max heart rate for about 30 minutes at least 3-4 times per week)
More conscientious eating (i.e. less saturated fats, less trans fats, less processed meats full of nitrites, less sugar, and more fruits and (green) vegetables rich in antioxidants, healthy oils (olive, avocado, etc.), and foods rich in nitric oxide (i.e. beets, spinach) – which help dilate the arteries
Nitric oxide is different from nitrites, which are typically used to preserve deli meats, and which have been proven to be carcinogenic
Sleep and stress management are critical as well, as too much stress can contribute to higher blood pressure, leading to greater inflammation, more plaque buildup, and a greater likelihood of soft plaques rupturing and causing a heart attack
Reducing alcohol consumption can help reduce blood pressure and reduce the risk of blood clots forming
Reducing smoking or the consumption of nicotine products, which deplete nitric oxide in endothelial lining cells, causing them to become stiffer and narrower, and increasing the risk of a blockage and thus a heart attack

In summary, one of the main ingredients to a long and healthy life is good cardiovascular health, which requires flexible, dilated arteries that allow for seamless, uninterrupted blood flow. While genetics play an important role on one’s predisposition to cardiovascular disease, this can be managed with a healthy, active lifestyle and – in certain cases especially as we age – modern therapies or interventions that help us better manage our cardiovascular health, such as preventive stenting or taking blood pressure reducing or cholesterol lowering drugs.


Comments